Introduction
With pharmacies of all types taking on more patient volumes than ever, interruptions are likewise becoming more frequent and more costly. But what is the true cost of interrupted work in pharmacy settings?
The cost of these interruptions isn’t just financial. While interruptions can’t always be avoided, increased instances of distraction can lead to greater cognitive demand and stress on pharmacists. In turn, this stress can increase their risk of errors on the job. Over time, these factors can contribute to burnout, poor job satisfaction, and increased turnover. All of which can be incredibly costly for pharmacies and health systems.
In this article, we identify several of the most common causes of interruption in the pharmacy. Next, we set out to discover the true toll of interrupted work on pharmacists, pharmacy employees, and their patients. We close by sharing a few best practices to reduce interruptions to promote pharmacist satisfaction and patient safety.
Common causes of interrupted work in pharmacy
Pharmacists experience as many as 13 interruptions every hour. According to an observational study published in the National Library of Medicine, five of the most common categories of interruptions to pharmacist tasks include patients, technicians, self-initiated, technology, and second pharmacist. Below, we break down each of these categories in more detail.
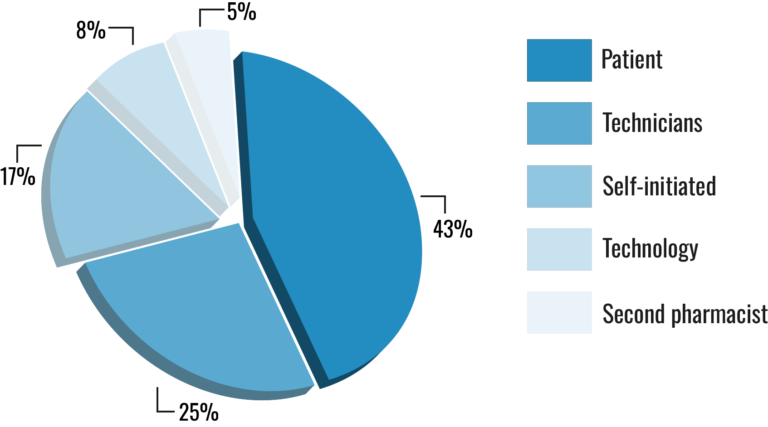
- Patient interruptions
Patient interruptions accounted for 43 percent of observed interruptions in the study. These included, for example, when a patient approached the pharmacy counter, drive-thru window, or called in to speak with a pharmacist. - Technician interruptions
The second most common type of interruption was by technicians and occurred in 25 percent of instances. These interruptions largely occurred due to technicians lacking the legal authorization to counsel patients on their medications. In addition, technicians interrupted pharmacists for assistance with prior authorization and prescription transfers. Technicians also initiated interruptions to discuss non-work-related topics. - Self-initiated
17 percent of interruptions were self-initiated by the pharmacist. The most typical example of this occurred when a pharmacist needed to call a physician’s office to retrieve missing information on a prescription. Additional examples include task coordination, management of other employees, and interruptions to discuss non-work-related topics.
- Technology
Eight percent of disruptions resulted from technology, including suboptimal technology workflows requiring frequent pharmacist intervention. Phone calls from within the building, such as through a PA system, were also a source of interruption. - Second pharmacist
Lastly, five percent of interruptions were due to the intervention of a second pharmacist. This includes, for example, when pharmacists change shifts and must communicate information about unresolved prescription issues. In addition, this occurred when pharmacists with technical questions sought a second opinion from another pharmacist.
What is the cost of interrupted work in pharmacy?
The financial cost
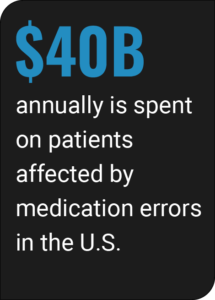
While it can be difficult to quantify the financial cost of interrupted work in pharmacy, interruptions may be a significant driver of costly medication errors. For example, the U.S. spends more than $40 billion annually on patients affected by medication errors. Preventable errors account for $21 billion of this total.
Interruptions are often necessary to communicate important information and even prevent medication errors. However, excessive interruptions place a high cognitive demand on pharmacists which can reduce the quality of their work and their well-being.
To illustrate, pharmacists are constantly switching between tasks due to interruptions. It is well-researched that rapidly multitasking in this way makes individuals more stressed, more distractible, and more prone to errors. In a pharmacy setting where patients’ lives are at stake, errors can be costly not only when prescriptions must be refilled, but when prescription errors compromise patient safety and outcomes.
Additional costs
When the effects of interruptions compound over time, they can lead to increased stress and burnout among pharmacists. A 2022 systematic review of over 11,000 pharmacists found that 51 percent are affected by burnout. When burnout grows more severe, turnover among pharmacists does as well. 80 percent of pharmacists surveyed by Pharmacy Times reported that they have considered an alternate career path.
The possibility of a mass exodus of pharmacists from the industry as indicated by this survey would come with catastrophic costs. Fewer community pharmacists could create gaps in patient care and widen existing gaps in economically disadvantaged and rural areas. As high-value healthcare providers, pharmacists leaving the industry would be taking their significant monetary value along with them as well.
Reducing pharmacy interruptions
Patient interruptions
Pharmacists of course aim to provide the best possible care and customer service to their patients. That said, it can be difficult to minimize patient interruptions in the pharmacy. One way to reduce patient interruptions is to train technicians to greet patients first and handle most tasks without the need to interrupt the pharmacist on duty.
Another solution is to keep two pharmacists on staff when possible. According to the same study referenced above, patient interruptions were less common in pharmacies with two pharmacists on staff. In these settings, one pharmacist can focus solely on assisting and counseling patients at the counter or drive-thru. In contrast, the second pharmacist can focus on verifying prescriptions with fewer interruptions.
The study also noted that the layout of the pharmacy may have led to fewer disruptions as well. Researchers observed that pharmacists working at a second counter behind the front counter, rather than directly in front of patients walking into the pharmacy, were better able to focus on their tasks with less interruption.
Technician interruptions
When it comes to the second most common type of disruption, technician disruptions, it’s critical to ensure that technicians are adequately trained to reduce the likelihood of an interruption during the workday. Again, technicians should be trained to handle most requests without the pharmacist. In addition, they should be able to recognize safety-critical tasks and initiate interruptions at the least disruptive time possible.
The color of the counter spaces within the pharmacy may even reduce technician disruptions as well. One study found that implementing a zero-distraction “red zone” counter space for medication preparations reduced team interruptions by over 40 percent. Adding visual cues like this to the pharmacy environment can help teams discern when interruptions are or are not appropriate.
It’s important to note as well that technicians already work hard to prevent interruptions from reaching the pharmacist. This includes processing prescriptions, answering phone calls, greeting patients, and more. Optimal training can ensure that their workflow is minimally disruptive to pharmacists performing critical tasks.
Other interruption types
The final three disruptions, self-initiated, technology, and other pharmacist, represent about one-fourth of the total disruptions observed in the study. Self-disruptions were most likely to occur when a pharmacist sought additional information about a prescription. This can be avoided or reduced by ensuring that pharmacists have ready access to patient health records.
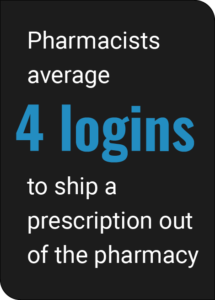
This potential fix relates to technology interruptions as well. According to an internal poll, we found that pharmacists average about four logins to ship a prescription out of the pharmacy. By redesigning technology workflows to be more efficient, pharmacy teams can prevent interruptions from clunky workflows. Prioritizing technology solutions that integrate with EHR systems can further help prevent interruptions resulting from a lack of patient information.
Conclusion
Interruptions are incredibly common in pharmacies and increasingly so as they struggle to maintain adequate hiring. Frequent disruptions can be costly not just financially, but to pharmacists’ mental well-being and performance as well. Increased interruptions can lead to greater stress and burnout, which contributes to higher rates of medication errors in addition to industry turnover.
These costs can be avoided by implementing the above evidence-based strategies in addition to prioritizing pharmacist and employee well-being. Investing in these measures now can reverse the costly trend of interruptions that pharmacists currently face. In addition, fewer interruptions and better job satisfaction among pharmacists can also promote patient safety and optimal patient outcomes.
About VPL Rx
VPL Rx is a clinically minded shipping, tracking, and compliance solution designed to modernize pharmacy distribution and promote healthier patients. Our quicker shipping workflow delivers prescriptions safely with real-time tracking, delivery alerts, and last-mile intervention. Exportable performance reporting and data analytics help pharmacies optimize costs and maintain compliance and accreditation.